Abstract
Introduction:
The most effective chemoimmunotherapy (CIT) in previously untreated CLL is the combination of fludarabine, cyclophosphamide and rituximab (FCR). Ibrutinib (I), the first irreversible inhibitor of Bruton's tyrosine kinase approved for CLL, has improved outcomes in numerous clinical trials compared to different CIT.
Methods:
FLAIR (ISRCTN01844152) is an ongoing, phase III, multicentre, randomised, controlled, open, parallel group trial for previously untreated CLL requiring therapy according to the IWCLL 2008 guidelines. Patients over 75 years or with >20% 17p-deleted cells were excluded. Participants were randomised on a 1:1 basis to receive 6 cycles of FCR (oral fludarabine 24mg/m 2/day for 5 days, oral cyclophosphamide 150mg/m 2/day for 5 days with IV rituximab [375 mg/m 2 on day 1/2 of cycle 1; 500 mg/m 2 on day 1 of cycles 2-6]) every 28-days or IR (Ibrutinib [420mg/day] plus rituximab [6 doses as for FCR]) given for up to 6 years with stratification by disease stage, age, gender and centre. The primary endpoint was to assess whether IR was superior to FCR in terms of investigator-assessed PFS. Secondary endpoints included overall survival,; attainment of undetectable MRD; response to therapy; safety and toxicity; health-related quality of life and cost-effectiveness. A formal interim analysis was planned when 191 events were observed in both arms or 109 events in the FCR arm alone with a p-value of 0.005 leading to reporting of the trial. Here we report the results of this planned interim analysis.
Results:
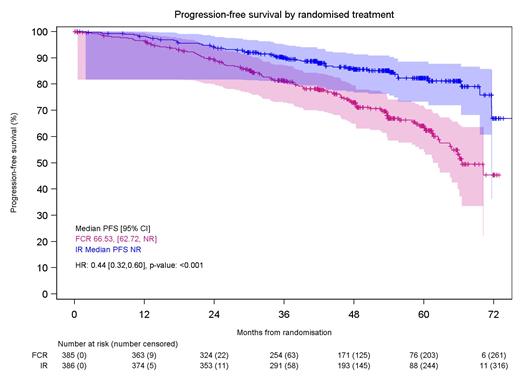
A total of 771 patients were randomised (385 to FCR and 386 to IR) from 113 UK Centres between 9/19/2014 and 7/19/2018. The data was locked on 5/24/2021. 73.3% were male, median age was 62 years (33.6% >65yo) and 45.1% were Binet Stage C. IGHV data was available for 728 (94.4%) patients with 53.2% IGHV unmutated (≥98% homology to germline), 40.5% IGHV mutated and 6.3% Subset 2. Hierarchical FISH testing revealed 0.4% 17p del, 15.4% 11q del, 12.3% trisomy 12, 29.7% normal and 35% 13q del; with 7.1% failed. The arms were well-balanced for disease variables with no significance differences. Median follow-up was 52.7 months. IR had a superior PFS compared to FCR (Median PFS not reached for IR versus 67 months for FCR; HR: 0.44; p<0.001; see Figure). The PFS was significantly better for IR in patients with IGHV unmutated CLL (HR: 0.41; p<0.001), but not for patients with IGHV mutated CLL at this follow-up (HR: 0.66; p=0.179). There was no difference in overall survival between the two arms (HR: 1.01; p=0.956) with a total of 29 deaths in FCR arm (including 4 from CLL, 3 Richter's [RT], 3 AML/MDS, 3 COVID-19 and 2 cardiac/sudden) and 30 in the IR arm (including 3 CLL, 1 RT, 0 AML/MDS, 3 COVID-19 and 8 cardiac/sudden). Second line treatment was initiated for 59 patients after FCR (including 38 BTKi, 7 venetoclax+R [venR], 4 BendamustineR [BR] and 3 CHOP-R [RT]) and 21 after IR (including 7 FCR, 5 venR, 1 BR, 1 CHOP-R [RT], 1 ABVD [Hodgkin's]). Overall, 88.1% of patients have received targeted therapies for CLL progression after FCR. The overall survival with FCR in FLAIR is significantly improved compared to FCR in previous NCRI trials (ADMIRE and ARCTIC) which had the same inclusion criteria, the same Centres and an identical FCR schedule, but were conducted prior to widespread availability of targeted therapies in the relapse (recruited between 2009 and 2012). The 4 year overall survival for FCR in FLAIR was 94.5% compared to 84.2% for FCR between 2009 and 2012. SAEs were reported in 53.7% of patients on FCR and 53.4% on IR. Notable differences for SAEs by organ class for FCR vs IR: infections in 33.6% of patients vs 27.1%; blood and lymphatic in 19.8% vs 10.7%; and cardiac in 1.1% vs 8.3%. With current follow-up, there were 10 sudden or cardiac deaths: 8 IR and 2 FCR. Further analysis indicated that 7 of the 8 cardiac or sudden deaths in the IR arm had a history of hypertension or cardiac disease (further detailed in additional abstract; Munir et al.). Neither of the sudden deaths in the FCR arm had a prior cardiac or hypertensive history or were on cardiac or anti-hypertensive treatment. There were 6 cases of secondary MDS/AML in the FCR arm and 1 in the IR arm.
Conclusion:
Ibrutinib plus rituximab resulted in a superior PFS compared to FCR. There was no difference in overall survival, most likely due to effective second-line targeted therapy in patients progressing after FCR.
Hillmen: Janssen: Honoraria, Other: Travel, Accommodations, Expenses, Research Funding; AbbVie: Honoraria, Other: Travel, Accommodations, Expenses, Research Funding; Pharmacyclics: Honoraria, Research Funding; Roche: Research Funding; Gilead: Research Funding; SOBI: Honoraria; BeiGene: Honoraria; AstraZeneca: Honoraria. Bloor: Novartis: Honoraria; Kite, a Gilead Company: Honoraria. Broom: AbbVie: Honoraria; AstraZeneca: Honoraria; Janssen-Cilag Ltd: Honoraria; Takeda UK Ltd: Honoraria; Celgene Ltd: Honoraria; Gilead: Honoraria. Furtado: Abbvie: Other: Conference support. Morley: Kite: Honoraria; Janssen: Honoraria; AbbVie; Takeda: Other: Conference support; Roche: Membership on an entity's Board of Directors or advisory committees, Other: Conference support. Cwynarski: Adienne, Takeda, Roche, Autolus, KITE, Gilead, Celgene, Atara, Janssenen: Other. Paneesha: Celgene: Honoraria; Roche: Honoraria; Janssen: Honoraria; Gilead: Honoraria; Bristol Myers Squibb: Honoraria; AbbVie: Honoraria. Howard: Roche: Current Employment. Cairns: Merck Sharpe and Dohme: Research Funding; Amgen: Research Funding; Takeda: Research Funding; Celgene / BMS: Other: travel support, Research Funding. Patten: NOVARTIS: Honoraria; ROCHE: Research Funding; JANSSEN: Honoraria; ASTRA ZENECA: Honoraria; ABBVIE: Honoraria; GILEAD SCIENCES: Honoraria, Research Funding. Munir: F. Hoffmann-La Roche: Consultancy; Alexion: Honoraria.